The following document was written by Mr Vik Veer MBBS(lond) MRCS(eng) DoHNS(eng) in Dec 2007. You may use the information here for personal use but if you intend to publish or present it, you must clearly credit the author and www.clinicaljunior.com
This site is not intended to be used by people who are not medically trained. Anyone using this site does so at their own risk and he/she assumes any and all liability. ALWAYS ASK YOUR SENIOR IF YOU ARE UNSURE ABOUT A PROCEDURE. NEVER CONDUCT A PROCEDURE YOU ARE UNSURE ABOUT.
Examination of the Cranial Nerves
The following document is one way of examining the cranial nerves. There are obviously many ways and techniques to do this which aren't mentioned here. I suspect you will only use this as a guide to your own examining technique which you should evolve to suit your own approach and style. I have also assumed that you have some knowledge of medicine throughout this examination. If you are uncertain to the reasons why i have mentioned things in my examination or need clarification there are some excellent books you can refer to.
I have written this with the idea that this will be used in an exam setting - so you will be presenting your findings as opposed to a clinic setting. i would try and talk constantly whilst examining the patient. It keeps the examiner interested and shows off what you know.
Introduction
introduce yourself and explain what you would like to do, then ask for permission.I Olfactory Nerve
"Have you noticed any change in your sense of smell?"
Testing formally involves using smells such as coffee, peppermint, vanilla in each nostril separately. Remember that noxious smells can be picked up by the trigeminal nerve. If the patient claims they cant smell anything ask them if they are able to smell petrol (trigeminal nerve)II Optic Nerve
Visual acuity use a Snellen chart 6 meters away, and with each eye separately find the smallest line of print that the patient can read. Allow the patient to wear glasses if they have them. Record the results (6/18 = at 6 meters the patient is only able to read print that normal can be read at 18 meters.)Colour Vision 15 Ishihara test plates at 75cm from the patient. 13+/15 is considered to be normal. If you want to try an online version try this Visual Inattention stand a meter away and then hold up both your index fingers 50cm away from both you and the patient. Make sure that your fingers are separated approximately by the width of your shoulders and that the patient is staring at your nose only. Then move each finger and ask the patient to call out if he/she can see them moving. In parietal lobe lesions (particularly in the non-dominant hemisphere) a isolated stimulus is perceived however it is missed when a comparable stimulus is presented contralaterally.
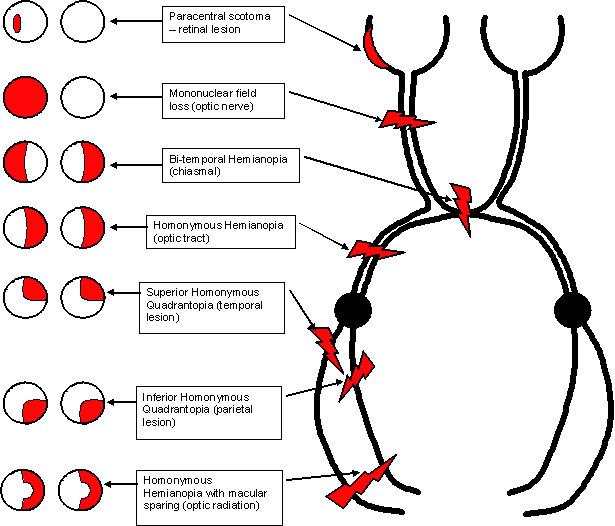
Visual Fields sit 1 meter from the patient, eyes level, and ask him to close one eye (you do the same) then put your hand to the extremes of your vision in the four quadrants (NE, SE, NW, SW) and move in towards the center until the patient can see it. Use a moving index finger for the outer visual fields and make sure that the patient's eye remains fixed on your own. To assess central visual field defects use a small coloured object as the moving finger is too crude. Start by assessing the blind spot and then scan over the central area on each eye.
Fundoscopy
III - Oculomotor, IV Trochlear, VI Abducens
- Note the position of the eye lids comment on any ptosis. Assess fatiguability by asking the patient to stare upwards (myasthenia gravis).
- Pupils Inspection "The are of normal size, shape, and are symmetrical" (Anisocoria - irregular size between the pupils - slight difference in 20% of the population. )
- Light reflex Always check that both pupils constrict on shining light into one eye.
- Swinging light test testing pupillary light response.
- Relative afferent pupillary defect is when shining light into the affected eye gives no reaction whereas shining light into the non-affected eye causes both to constrict. Going back and forth should keep the pupils constricted, but not with this defect.
- Relative efferent pupillary defect is when you shine light into the affected eye there is no direct effect except there is a consensual constriction in the other pupil. Shining light into the non-affected eye constricts it but there is no response on the affected side.
- Accommodation Reflex ask the patient to fixate on a far object and then quickly on a near object you should see a constriction of the pupil with this manoeuvre.
Abnormalities
Horner's syndrome - unilateral pupillary constriction, slight ptosis, enophthalmos, (sweating on the affected side of the face.Argyll Robertson Pupil - small irregular pupil which is not reactive to light but will have a accommodation reflex. (tip to remember - think of 'she's a prostitute - she'll accommodate - but she won't react')
Holmes-Adie pupil (myotonic)- large pupil with a sluggish reactions to light and accommodation. Associated with absent tendon reflexes in women.
Eye Movements
- Try and make a large H shape with your finger and get the patient to follow it. Basically you should be trying to force the patient to use all the muscles of eye movement and easily pick up any diplopia. Different clinicians use different shapes.
- Cover testing ask the patient to fixate on an object (your nose) and then cover an eye and then remove it to see if the covered eye got lazy and wandered off - you can tell from different types of squint / strabismus and lateral rectus muscle problems.
- Saccades - rapid shifts in position of the gaze assessed by asking the patient to follow a swiftly moving target. Optokinetic movements are when the eye follows a repeating target (like on the underground and looking at the signs outside)
- Head thrust test - is a test of the vestibulo-ocular reflex. Hold the patients head with both hands and ask them to constantly stare at your nose. Then quickly twist / rotate the head to one side and watch the eyes. In normal people the eyes continue to fixate on your nose no matter how fast you go. If you see saccadic movements of the eyes as they try and recenter themselves then there is a defect in the vestibulo-ocular reflex.
"if you could please follow my finger with your eyes and keep your head still, and let me know if you notice any double vision"
Abnormalities
Nystagmus an involuntary rhythmical oscillatory movement of the eyes.- Pendular nystagmus back and forth movements are of equal velocity. Usually a congenital defect
- Jerk nystagmus slow drift of eye with rapid saccadic movement to correct the drift.
- 1st degree - present only with the eyes looking in the direction of the fast component.
- 2nd degree - persisting even when the eyes are looking straight ahead.
- 3rd degree - persisting even when the eyes are looking in the direction of the slow component.
- Internuclear Ophthalmoplegia lateral and medial rectus muscles are harmonised by the medial longitudinal fasciculus which links the abducens nucleus in the pons with the contralateral medial rectus part of the oculomotor (III) nucleus in the midbrain. A lesion here results in a successful abduction on attempted lateral gaze but a failure of the adduction of the other eye with nystagmus in the abducting eye. This lesion may also give a skew deviation in which one eye is elevated relative to the other. This is most commonly found in MS.
- III nerve palsy ptosis (paralysis of the levator palpebrae superioris), no pupillary responses (fixed and dilated). The eye is also stuck in the 'down and out' position.
- IV nerve palsy difficulty in looking down (walking down stairs)
- VI nerve palsy unable to abduct the eye.
V Trigeminal Nerve
Motor component- Look for wasting of the muscles of mastication - "Clench your teeth for me please" feel the masseter and temporalis.
- Ask the patient to loosely open their mouth (notice any jaw deviation). Use the tendon hammer on the chin for the jaw jerk.
- Compare the light touch sensation between the ophthalmic, maxillary, and mandibular zones of the trigeminal nerve.
- Corneal reflex touch the corner of the eye, with a wisp of tissue no menace reaction if possible.
VII Facial nerve
"have you noticed any change in your sense of taste?"
- formal testing would involve using sweet, sour, salt on the anterior 2/3 of the tongue."have you noticed that noises seem excessively loud in one ear rather than the other?"
facial nerve supplies the stapedius muscle of the middle ear which reduces conduction of very loud noises through the ear."Do any of your eyes seem dry to you?"
facial nerve provides innervation (at least part of the way) of the lacrimal gland which produces tears.Muscles of facial expression
lift your eyebrows high in the air frown squeeze your eyes shut don't let me open them
(try and open their eyes with your fingers they should be strong enough to resist you)Show me all your teeth - blow your cheeks out
(no air should escape through the lips on maximal inflation)Abnormalities
Lower motor neuron facial weakness global weakness of one side of the face.Upper motor neuron facial weakness the frontalis muscle is normally unaffected as it has a dual nerve supply from both hemispheres.
VIII Vestibular/Cochlear Acoustic Nerve
- (see Ear examination for more detail) Auditory function test each ear separately by rubbing your fingers together or listening to your watch tick. Rinne's test use a 512 Hz tuning fork and place it on the mastoid process and then again near the pinna ' Where does the tuning fork sound loudest, here or here?"Weber's test place the same fork at the midline vertex and ask "Which ear can you hear the tuning fork in, or are they both the same?"
With sensorineural hearing loss the sound is heard more in the non affected ear. With conductive loss the sound localises on the affected side.
Vestibular function
"do you experience any vertigo or dizziness when you get dizzy does the world is spin around you?"
- Hallpike Manoeuvre gently but rapidly lie the patient down over the side of the bed and turn their head to the right - hold the patient there for at least 20 seconds and check the eyes for any nystagmus. Repeat the test but this time drop the patient to the left.
- Rombergs test ask the patient to stand, feet together and eyes closed. If they have a problem they tend to fall over on the same side of their lesion.
- Unterberger test ask the patient to march on the spot with arms stretched out infront and eyes closed. A abnormal vestibular system will result in the patient rotating greater than 30 degrees toward the affected side.
IX Glossopharyngeal Nerve
"For the glossopharyngeal nerve I would test the gag reflex by placing an orange stick on the posterior wall of the pharnyx and watch for the palate to rise in the midline".
try and avoid doing this in the exam as it isnt pleasant for the patient.X Vagus Nerve
"Would you swallow some water for me please"
"Say 'Ah' for me please"
the palate and the uvula are pulled up equally. Also you can notice any dysphonia from paralysis of either of the recurrent laryngeal nerves.XI Accessory Nerve
Inspect for any muscle wasting.Turn your head left and right
(hold their chin to test power). (Testing power of the sternocleidomastoid muscles)"Shrug your shoulders up - don't let me push them down"
testing the trapezius.XII Hypoglossal Nerve
"Stick your tongue out for me."
Tongue leans towards the defective side.Completion
Ask to complete the neurological examination by testing the peripheral nerves and any other system if you think this is relevant.There are very good online guides for this subject - such as:
- www.clinicalexam.com
- The Precise Neurological Exam
- NEUROLOGICAL EXAMINATION (R. Duncan Kirkby, Ph.D. © 2002)
- Student BMJ
- Utah library
- University of Dundee