The following document was written by Mr Vik Veer MBBS(lond) MRCS(eng) DoHNS(eng) in Dec 2007. You may use the information here for personal use but if you intend to publish or present it, you must clearly credit the author and www.clinicaljunior.com
This site is not intended to be used by people who are not medically trained. Anyone using this site does so at their own risk and he/she assumes any and all liability. ALWAYS ASK YOUR SENIOR IF YOU ARE UNSURE ABOUT A PROCEDURE. NEVER CONDUCT A PROCEDURE YOU ARE UNSURE ABOUT.
FOREIGN BODIES - THROAT
History is rather important here. A history that would alert you would be one of eating a bony fish or other meat and suddenly there is an inability to swallow with clearly localised pain. These patients tend to look like they are choking and are in extreme distress. They also are unable to swallow their own saliva and so spend much of their time spiting to avoid swallowing. A history of this happening before and progressive difficultly in eating is also important here. These patients can anything stuck including bone, meat boluses, etc.
Another more common history is one of someone eating some fish or chicken and experiencing pain suddenly on swallowing. They might even vomit but in the end they are generally alright except they feel a vaguely localised pain every time they swallow. They are able to eat and drink if forced, but it hurts and it worries them terribly. This history is at the opposite end of the spectrum and these patients are more likely to have had a small scratch in the mucosal lining of the upper oesophagus or above.
Obviously there are a lot of people whose history lies between these two extremes and all of these patients could have a foreign body trapped. Experience and careful examination and investigation will tell you which patient, have and which donít have a foreign body.
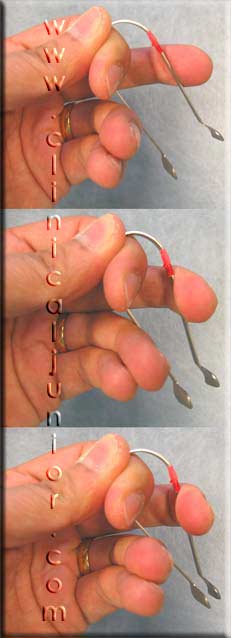
Firstly most bones tend to lodge themselves in the tonsils or base of tongue. Therefore all patients should have their oral cavities examined very closely for the very thin bone that can lurk here. These bones can be so thin that they can be mistaken for a strand of saliva. Look carefully and rule everything out. If you can see a bone in this area then remove it with a magillís forceps or a burkittís straight forceps (anything you feel comfortable and confident with), being careful not to cause more damage to the surrounding mucosa.
If you are finding it hard to see the base of the tongue you can lie the patientís head over the side of a bed and look as an anaesthetist would with a curved laryngoscope. Remember to press down on the base of the tongue to suppress the gag reflex (you can also use xylocaine spray).
If you canít see anything here and you are confident there is something there you can move on to flexible fibreoptic nasendoscopy to look more closely. Special hiding places would be the vallecula or the piriform fossae that can harbour these bones. Even though not specifically designed for viewing the oesophagus you can view the upper oesophagus with the nasendoscope by following the piriform fossa posteriorly and asking the patient to swallow the scope. This canít be tolerated by all and requires some experience and knowledge of the anatomy. The rule is not to advance unless you can see where you are going.
If you see a bone below the level of the base of the tongue then the patient will need a anaesthetic to remove it.
The question about doing a lateral x-ray is controversial. Some say that these radiographs are so difficult to interpret, that they shouldnít be done. Certainly they shouldnít be done in the case of swallowing bones that do not show up on x-rays (mainly the cartilaginous type bones). The heterogeneous calcification of the cartilages of the larynx can fool even experienced radiologists, and if you are certain there is a bone there you should progress to a CT scan.
If you have searched thoroughly and are now certain there is no foreign body you can send these patients home with analgesia (paracetamol and NSAIDs) with amoxicillin if you think it is an infected case.
If you think the patient has a meat bolus that they canít swallow you should try the following therapies:
- If they manage to swallow a little fluid try them on a carbonated drink (coke etc.) It seems that when patients belch it can dislodge a meat bolus.
- Try buscopan 20mg and again 30 minutes later with 5mg of diazepam to relax the muscles enough so they can swallow the bolus.
- Admit the patient overnight as sleeping can sometimes allow the bolus to pass
- If none of these work, they will need an anaesthetic to remove the bolus.
Further Reading
eMedicine - Esophagus, Foreign Body : Article by Veronica Rooks
Esophageal foreign bodies
American Family Physician, by Keith M. Ratcliff
FOREIGN BODIES Ė EAR
This usually occurs in children. You only get one chance to remove a foreign body from a childís ear without GA. If you are not confident then donít attempt it, leave it for someone who will remove it first time.
It is normally safe for the patient to go home (as long as there is no florid infection, etc.), and can return to be seen the following day in the ENT Emergency Clinic or local alternative.
Live insects stuck in the ear can be killed by drowning it in eardrops and then removed.
Do not use water to syringe out vegetable products from the ear as they will swell and cause pain and sometimes damage.
A battery in the ear requires removal ASAP Ė please contact the ENT team for an emergency operation.
Further Reading
eMedicine - Ear Foreign Body Removal : Article by Angela On-Kee Kwong
ncemi.org - Foreign Body in Ear
FOREIGN BODIES Ė NOSE
This usually occurs in children as adults are normally able to remove it themselves. You only get one chance to remove a foreign body from a child without GA due to agitation.
Different departments have different views about admitting these children as there is a theoretical risk of aspiration. If they arenít admitted they should be booked in the next day (starved) to see the ENT team. Please ask the parents to make sure the child is NBM.
A battery in the nose requires removal ASAP Ė please contact the ENT SHO