The following document was written by Mr Vik Veer MBBS(lond) MRCS(eng) DoHNS(eng) in Dec 2007. You may use the information here for personal use but if you intend to publish or present it, you must clearly credit the author and www.clinicaljunior.com
This site is not intended to be used by people who are not medically trained. Anyone using this site does so at their own risk and he/she assumes any and all liability. ALWAYS ASK YOUR SENIOR IF YOU ARE UNSURE ABOUT A PROCEDURE. NEVER CONDUCT A PROCEDURE YOU ARE UNSURE ABOUT.
EPISTAXIS





Apart from the elderly, the anterior nasal septum, (Little’s bleeding area) is the commonest place to bleed from as it is the centre of a large confluence of end-arteries. This area is also called Kiesselbach’s plexus. Another very common area to bleed from is Woodruff’s plexus which is far more posteriorly located in the nose. It lies quite deep within the nasal cavity on the lateral surface which is also the location of the sphenopalatine artery (1cm inferior and 1cm anterior to the posterior margin of the middle turbinate). The elderly are more commonly affected with posterior bleeds.
The causes of epistaxis are mainly:
• Nose picking
• Exposure to cold (reduced temperatures disrupt cillary action) dry air
• Tumours
Hypertension has not been shown to cause epistaxis – however, those with high blood pressure tend to bleed more and recur more frequently than those without.
Management
The condition is normally self-limiting with First aid. This consists of pinching the soft part of the nostrils tightly against the septum for at least ten minutes without a pause. Pinching the end of the nose should be shown to the patient – remind them that pinching the upper bony bridge part of the nose will not achieve anything.Whilst pinching the nose ask the patient to suck on ice (freezing the greater palatine artery that runs along the roof of the mouth), and lean forward. By leaning forward the patient is less likely to swallow any blood. Ensure that they spit out all the blood that runs back into the post nasal space. If they are continuing to bleed even whilst pinching the nose they may have a posterior bleed which can’t be treated with first aid manoeuvres.
With a more significant bleed your first priority is to make the patient safe. Resuscitate. Insert large sized intravenous cannula and replace lost fluid. If a heavy bleed, group and save for possible blood transfusion.
In your history ask about anticoagulant therapy (including Aspirin), or haematological disorders. In those who are on aspirin or warfarin – do not stop these drugs unless the INR is grossly elevated and therefore the cause of the bleed. In those with a coagulation defect try and correct this problem first as you’ll find that attempting to manage these bleeds with packing or cautery tends to make the situation worse (as it causes more trauma to the nasal mucosa which makes the bleeding worse). Correcting the coagulation defect medically normally stops this kind of bleeding. Obviously this is not always appropriate in the case of a massive bleed but should be kept in mind that the only real problem is the coagulation rather than the bleed itself.
Be mindful that hypertension makes epistaxis worse and difficult to control. Controlling a grossly elevated hypertension is an important consideration if not associated with stress or pain.
In those who aren’t controlled with first aid then one may require other avenues of treatment. Wear gloves and apron and have a headlight, thudicums speculum (see picture and also how to hold it!), local anaesthetic spray (xylocaine - see picture), yanker sucker (see picture), and silver nitrate sticks (see picture of stick and the chemical tip).
Look inside the nose and suck out the blood with the yanker sucker and try and identify the bleeding point. You will notice what appears to be bleeding from ‘old’ blood in the post nasal space. Sucking this blood out with the yanker sucker or helping the patient spit it out can resolve this issue.
Once you have found the bleeding point in the anterior part of the nose spray it with xylocaine and allow the patient to spit it out (tastes disgusting!)
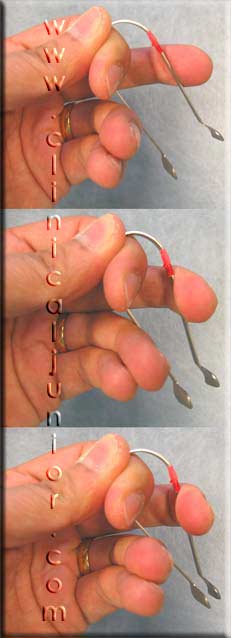
Make sure the area is anaesthetised by waiting for a few minutes and then carefully hold the black end of the silver nitrate stick (see picture) firmly against the bleeding spot for at least 30 seconds.
Do not move it around or roll it, just hold it there for 30 seconds and then reapply with another stick for another 30 seconds to gain control of the bleed. The area quickly goes first white and then black – this is normal.
A useful tip is to also cauterise the area directly around the bleeding point with multiple nitrate sticks with the same technique, controlling the feeding vessels.
Remember don’t cauterise a patient who is bleeding because of a coagulation defect – this will probably worsen the problem.
Don’t cauterise both sides of a septum as this can lead to a septal perforation with all it’s associated problems.
Once the bleeding has stopped give them Naseptin cream (contains peanut oil – ask about allergies - give Bactroban as an alternative) to be put in the nose twice a day for 2 weeks.
To put this in the nose you need to put a drop on the tip of the little finger and then placed very gently inside the entrance of the nose (do not rub inside the nose as this will cause bleeding). Then rub very gently on the outside of the nostril to direct the cream up the nose.
Some patients (mainly elderly) who have very dry and thin nasal mucosa could be advised to use Vaseline after the course of Naseptin to keep the muscosa moist and protected avoiding future bleeds.
The advice you give patients upon discharge is:
- Avoid hot drinks / meals for two weeks – clearly no one is going to follow this advice and so I sometimes say with each mouthful wash it down with ice cold water to keep the mouth cold.
- Avoid straining / heavy lifting / bending down (anything that could increase the blood pressure in your head.
- Don’t pick your nose – don’t rub your nose – don’t touch your nose. This can be likened to picking a scab.
- When sneezing – try and sneeze with your mouth open. Don’t blow your nose!
Certainly no one ever follows this advice, but a little is better than nothing.
There will be occasions when you are unable to see the bleeding point and therefore are unable to cauterise the patient. This is likely to be a posterior bleed (from woodruff’s plexus), which is on the lateral wall of the nasal cavity near the post nasal space.
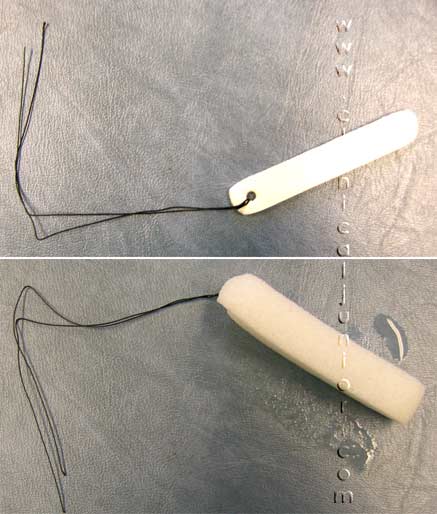
In this situation you will need to insert a merocel pack. This is a fancy tampon that is inserted into the nose to control the bleeding by direct pressure (see the picture of a merocel before and after expanding). The technique for this is to first remove all the blood with a yanker sucker from the nose and spray with local anaesthetic as before.
Then get a 10cm merocel pack and hold it tightly on the end which has a dark string attached to it. Holding the pack completely horizontally, push the pack into the nose straight back. Follow the floor of the nose and push along the septum of the nose. Do not push up the nose or you will get stuck. The patient will protest and it will seem horrible, but do it firmly and quickly and it should be all over in a second. Make sure the pack is inserted all the way in. There should be no pack visible outside the nose if inserted properly.
A common joke is the ‘walrus sign’ the (white merocel hangs out of the nose like a tusk) – try not to be at the receiving end of this joke.
Give the patient a break and check to see if the bleeding has stopped (check the back of the mouth incase it is trickling down the posterior pharyngeal wall).
If your department only has 8cm Merocel packs then make sure you push them as deeply as possible into the nose.
If your department is rich it will have Rapid Rhinos, which are inflatable balloons coated in a lubricant that will also stop bleeding. Current thinking is that they are no more effective than Merocels but they are far more comfortable to insert for both the patient and doctor. Just remember to put the pack in water for at least 30 seconds to ensure the lubricant is activated. Insert as before and when in place blow up the balloon with AIR (approximately 5 – 7mls).
Some people place a Merocel in both nostrils to ‘compress’ the septum in the middle. Since the bleeding tends to occur on the lateral wall in posterior bleeds this doesn’t make sense to me, but it is common practice for whatever reason.
Patients with a merocel pack insitu are almost always admitted to the ward for at least 24 hours. Follow the guidance in your own hospital – (very few departments allow these patients to be sent home).
 If the merocel pack doesn’t work you are now in more specialised territory and will require a more senior ENT / A&E doctor to help you. Typically these posterior bleeds require a small female urinary catheter to be placed in the post nasal space and then the balloon is blown up to stop blood going down into the oropharynx. Then with a Tiley’s forceps (see picture) BIPP is packed into the nose layer by layer until a few meters are inserted deeply into the nasal cavity. This can be dreadfully painful and traumatic if done without guidance the first time, ask a senior to help you.
If the merocel pack doesn’t work you are now in more specialised territory and will require a more senior ENT / A&E doctor to help you. Typically these posterior bleeds require a small female urinary catheter to be placed in the post nasal space and then the balloon is blown up to stop blood going down into the oropharynx. Then with a Tiley’s forceps (see picture) BIPP is packed into the nose layer by layer until a few meters are inserted deeply into the nasal cavity. This can be dreadfully painful and traumatic if done without guidance the first time, ask a senior to help you.
If this doesn’t work the patient requires an emergency operation (endoscopic Sphenopalatine artery ligation or maxillary artery ligation or even an external carotid artery ligation).
Further Reading
eMedicine - Epistaxis : Article by Jeffrey Evans, MD
Management of Epistaxis - January 15, 2005 - American Family Physician
eMedicine - Epistaxis : Article by William Gluckman